Digital Health Checks & Hormone Balances
Beyond the wellness trends, what is hormone replacement therapy and how can digital health help?
Hormones are all the rage. From cortisol levels to low-T to GLP-1s, it seems like everyone is talking about hormones these days. We’ve moved from casually discussing stress and metabolism to actively trying to “hack our hormones.” It’s a shift—not inherently good or bad—but one that suggests a growing desire to take control of our biology.
Lately, sex hormones have taken center stage, especially in digital health. Menopause—long a taboo topic—has finally broken into mainstream (digital) health discussions. At the same time, there’s been interest in testosterone therapy among women prompted by social media influencers and conflicting information about menopause hormone therapy. Menopause content has risen on TikTok, and over the past few years, hormone replacement therapy (HRT) has become a focal point for digital health startups.
What I want to explore here is how DTC companies have entered the HRT space and what that means for consumers. Additionally, I wish to ask how digital health can improve access and safety in HRT.
What is hormone replacement therapy?
Hormone replacement therapy (HRT) is used when the body doesn’t produce enough of a certain hormone to maintain normal function. Most commonly, HRT is prescribed to relieve symptoms of menopause by replacing estrogen and progesterone, which naturally decline during perimenopause and menopause. It is also essential in gender-affirming care for transgender and nonbinary people.
For menopause, HRT—or as it’s increasingly called, menopausal hormone therapy (MHT)—has been a topic of debate for decades. In 2002, The Women’s Health Initiative (WHI) study reported an increased risk of breast cancer, heart disease, and stroke linked to HRT (and that the risks outweigh the benefits), leading to a sharp decline in its use. In fact, a recent study found that use plummeted from 26.9% to 4.7% from 1999 to 2020.
However, a 2024 review of the WHI study reframed the conversation, emphasizing the importance of shared decision-making between patients and doctors. Authors underscored that the risks and benefits of HRT vary on an individual level–suggesting a need for personalized care.
Given this history, any digital health approach to MHT must take a measured approach to balancing access with safety…perhaps an individualized risk-benefit analysis.
Gaps in hormonal healthcare
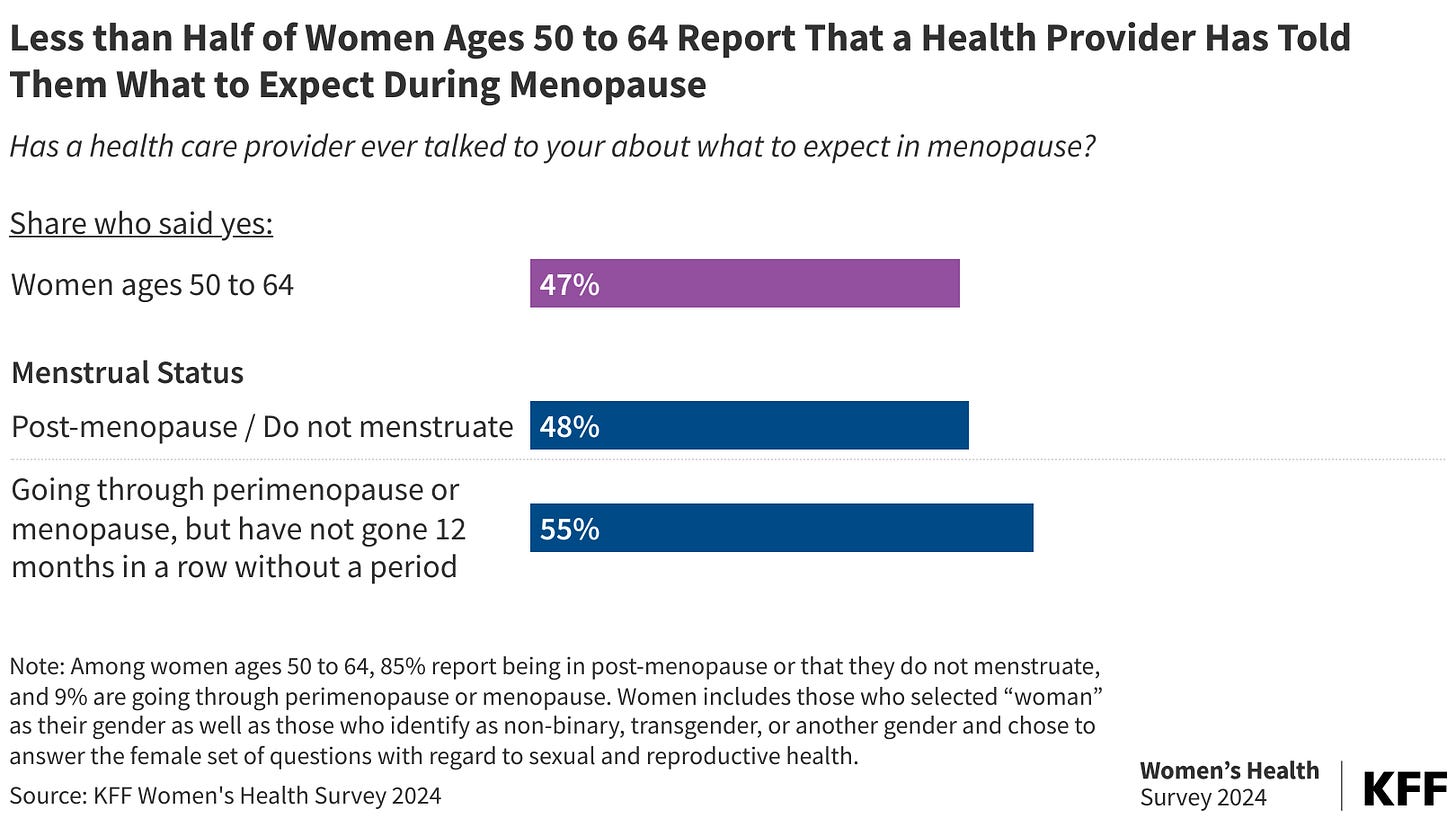
Despite the growing conversation around hormone health, actually accessing care is still a challenge—especially for menopause and gender-affirming care. Menopause care is still severely under-discussed. Fewer than 50% of women aged 50-64 have had a conversation with their doctor about menopause.
There are less than 2,500 certified menopause providers. OB-GYNs are key prescribers of MHT, yet training remains inadequate. A 2023 study found that only 31.3% of OB-GYN residency programs include menopause education (not that great of a jump from a 2013 study that found that it was 20.8%). Gender-affirming HRT faces even more barriers–not just from a lack of providers, but also due to stigma, insurance coverage gaps, and restrictive laws.
This is where digital health can play a critical role.
Digital health filling the gaps
With traditional healthcare not providing sufficient support, digital health companies have stepped in to address access. Companies like Noom and Midi now offer HRT directly to patients, aiming to reduce barriers like stigma and long wait times. Hims & Hers has expanded its at-home testing capabilities to include testosterone, perimenopausal, and menopausal support. And PfizerForAll now connects individuals seeking menopause care with healthcare providers.
But while these platforms increase access, they also shift more responsibility onto consumers. The issue isn’t just that women aren’t receiving care for menopause–it’s that they are often left to initiate treatment themselves. If doctors aren’t starting these conversations, should the solution be companies that rely on consumers to initiate treatment?
There’s a need. So let’s get it right.
The rise of DTC HRT raises an important ethical question: Are these platforms truly empowering consumers, or are they shifting too much responsibility onto them? For instance, some experts worry that DTC HRT may lead patients to skip in-person exams, where providers might detect underlying health issues beyond just hormone levels.
This need isn’t limited to menopause care. Gender-affirming hormone therapy also faces significant access challenges, with far fewer telehealth companies focusing on trans healthcare.
I’m not saying we shouldn’t use these platforms. I’m saying we should make them even better. If done right, digital health could improve HRT by combining it with wearables to detect hormonal fluctuations; ensuring ongoing monitoring and lab testing to ensure adequate follow-up care; AI-driven decision support to personalize and optimize hormone dosing.
The way we talk about hormones is changing–but how we deliver care needs to evolve, too. Access is SO important. But so is doing it right. In addition to asking, “how do we expand access?”, it’s also asking, “how do we do it safely?”
Share below how you see digital health shaping MHT and hormone therapy at large! What innovations (or risks) should we be thinking about??

