Zoom Zoom: From Mobile Apps to Mobile Clinics
Examining an important infrastructure powering care access
I’d like to explore a quite literal form of “direct-to-consumer” healthcare today: mobile health. And no, not the app that delivers Zoom-like telehealth. I’m talking about that zoom zoom kind. Vans. Buses. Clinics on wheels. With doctors (or not so much—I’ll get to that in a bit) aboard.
The post-pandemic hype around virtual care is stabilizing, and we know that tech alone can’t solve access. At the same time, rural hospitals are closing; provider shortages are deepening; reproductive care is vanishing across states. Mobile clinics are not novel by any means. But they feel newly urgent.
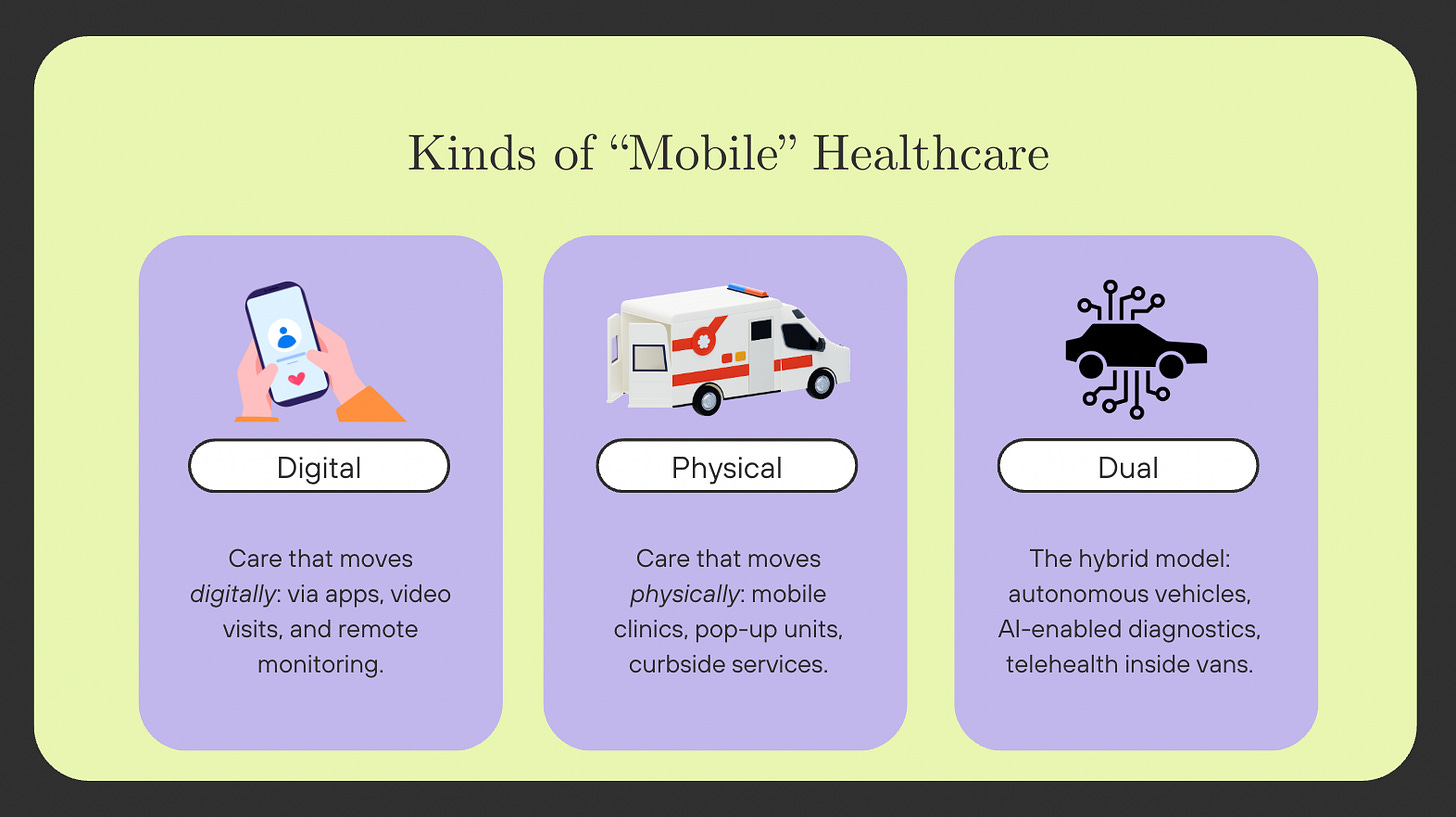
When you hear the term, “mobile health,” you probably picture some kind of healthcare app delivered through your phone. Part of the digital health, eHealth, mHealth universe—digitally mobile care. But recently I’ve been intrigued by physically mobile care. After all, “mobile” just means “capable of moving or being moved.” This detour into semantics is simply to highlight: mobility is infrastructure. Digital and physical infrastructure. This infrastructure determines access: the where and the how people get care.
Now, what kind of mobile solution is needed: device or wheels? Challenges that are commonly cited with implementing digital health solutions in rural areas include spotty internet connectivity and lack of access to specialists. As I explore below, as mobile clinics become increasingly tech-enabled, they should be on the radar of those in digital health.
Getting to the heartbeat of America
Coming out of the pandemic, we’ve sobered up from the excitement around telehealth. While virtual care is now ubiquitous, it is not a fix-all solution. For many, particularly those who are unhoused, living in rural areas without stable internet, or lacking privacy at home, telehealth is just not viable or reliable.
That’s where mobile clinics come in. They help improve access to care by reducing geographic and transportation barriers, adapt to the changing needs of communities, support continuity of care, and provide in-person and culturally competent care that builds trust.
There are an estimated 3,000 mobile clinics operating in the U.S.—you can explore them on the Mobile Health Map, which tracks where they are located and what services they provide.
In 2023, Congress passed the MOBILE Health Care Act, a pivotal piece of legislation that expanded the ability of community health centers to establish mobile clinics in rural areas and underserved communities. Previously, a permanent brick-and-mortar site was necessary to accompany a proposed mobile health clinic. But now, that requirement no longer exists. This act allows federal funds to be used to set up new mobile healthcare delivery sites. A very good example of the role of policy in improving access!!
Several studies have mapped out who mobile clinics are reaching and what they’re providing. A 2020 analysis of 800+ clinics found that 47% offered preventive services, 41% delivered primary care, and 28% provided dental care. Another 2020 study analyzed the operating costs of mobile clinics by service categories, and they found costs increase from mammography/primary care/preventive delivery to dental/preventive. But my main takeaway is that mobile clinics are trying to give people very necessary services and help ameliorate disparities.
However, limitations of mobile clinics include potential fragmentation of care, variable funding to support mobile clinics, constraints of space, and staffing difficulties.
Innovation that excites (me!)
There have recently been interesting applications and a breadth of services being delivered via mobile clinics. For example, for substance use disorder, the University of Maryland runs a mobile treatment unit that connects patients to an addiction medicine specialist via encrypted, HIPAA-compliant video conferencing. This is a great example of how mobile clinics can blend having a physical presence with telehealth support. In Portland, Oregon, mobile clinics operated by New Season are delivering opioid addiction treatment to unhoused individuals. Features include medication-assisted treatment, counseling on-site, and telemedicine. This is an extremely important way to solve a care gap for people who can’t access brick-and-mortar or telehealth care.
Following the overturning of Roe, mobile clinics were deployed for abortion access, parked along state borders. Around the time of the Democratic National Convention (DNC), Planned Parenthood set up a mobile clinic that provided vasectomies, medication abortion, and emergency contraception. In rural Texas, another mobile clinic provides access to long-acting reversible contraception (i.e., IUDs), which is a valuable strategy in areas with few OB-GYNs.
Last summer, Yale started offering mobile services including mobile pharmacy services. This enables having a doctor’s visit at the same place where you’d pick up your prescription.
And then, there’s the Dollar General case study. A few years ago, Dollar General partnered with DocGo to deploy mobile clinics in rural areas. The plan was to pilot different locations to understand the supply-demand dynamics of the area/community. After 18 months, the pilot program ended.
In theory, sure: bring healthcare to places people already go. But things didn't go well. It seems that there was some hesitation to seek care in the parking lot of a Dollar General store, with some questioning the motives behind parking these clinics outside a store…which could lead to more foot traffic into the store. I’d assume that parking these clinics outside more “trusted” locations like schools, churches, or community centers would have been better.
Going above and beyond
Not all mobile clinics are deployed to fill essential and lifesaving access gaps. Not all are trying to democratize access to care. In August 2024, Prenuvo tested out a mobile MRI clinic in Buffalo, NY. This is the same full-body MRI company that Kim Kardashian tried out. While this is meant to be preventive, it is preventive imaging for those who have a few thousand dollars that they are willing to pay. It seems like there are a few objectives here: raise consumer awareness of full-body MRIs and assessing which locations might justify a brick-and-mortar location.
The juxtaposition of preventative mobile MRIs for the rich versus opioid care vans for those unhoused is reflective of the profound inequalities that exist in healthcare; but also reflective of the fact that mobile clinics—whether luxury or lifesaving—are here to stay. Same model, different margins.
Healthcare’s ultimate driving machine
We’re getting closer to mobile clinics without a driver and without a doctor. Autonomous mobile clinics (AMCs) are self-driving vehicles outfitted with diagnostic tools, tablets, and AI-powered clinical assistants. Researchers at the University of Michigan are testing AI-enabled teams through mobile clinics that can screen for diseases, reduce overhead costs, and supervise “generalists” or those who might not know a certain procedure, almost like a virtual mentor.
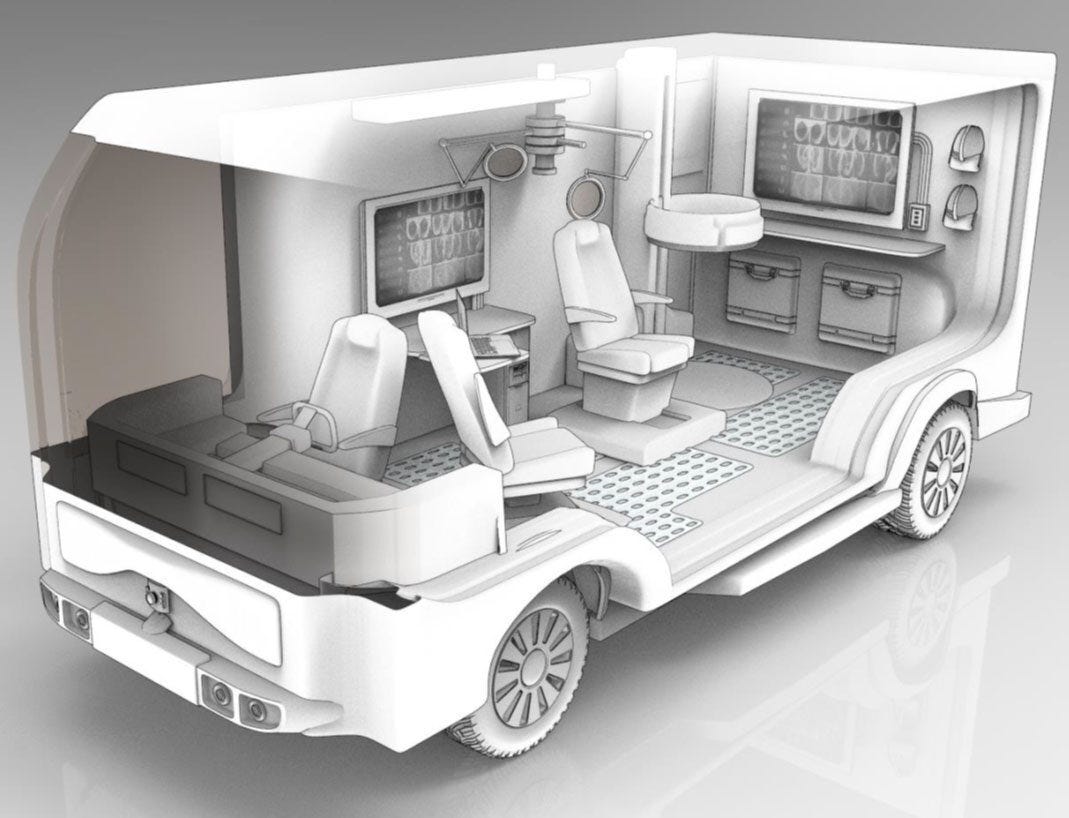
A lot of mobile clinics now integrate telehealth or digital tools onboard (like encrypted video consults, EHR connectivity, remote diagnostics), and this is just an extension of that. As we move from MHCs to AMCs, digital mobility + physical mobility intersect. As mentioned above, one of the limitations of mobile clinics is staffing difficulties and using AI, that is a limitation that could be overcome with AMCs.
And as someone who just saw five Waymos on the road in LA, the idea of a driverless clinic does not seem so wild.
Vorsprung durch technik
While there is Uber Health and Lyft for Healthcare, this is different. Those services help you get to care. Mobile clinics bring care to you.
Rural healthcare matters and the literal mobility of healthcare feels like an overlooked tool to help close the access gap. The integration of autonomous vehicles and AI doctors feels positive.
So, what does it mean to truly “bring care” to someone? I’m curious to know how you are thinking about how, where, and for whom care happens…because the road to equity might literally be on the road.
And since recession pop is so back, I’ll leave you with this bop: Vroom Vroom by Charlie XCX. You’re welcome.